Together at the Center
TOGETHER AT THE CENTER
A PFCCpartners and Camden Coalition Content Partnership
Join us October 15-17, 2025 in Portland, OR
Do you miss the annual PFCC Conference?
We do too! …and we miss you! Save the date!
Message from Stephen Hoy, Chief Operating Officer, PFCCpartners
It is in this moment of uncertainty across our health system that gives us great enthusiasm to announce a partnership with Camden Coalition. We are excited to convene passionate leaders improving person-centered care for all people.
The energy and inspiration that comes from being together [in-person] is something we miss dearly. I personally never recognized at the time just how much I was fueled by the annual dose of inspiration that would come from our PFCC Conference. But organizing the PFCC Conference “as it used to be” has been an enduring challenge for our small team, which has led us to seek new opportunities to convene our community.
So, in the spirit of coming together to meet this moment, PFCCpartners will be a valued content partner at Putting Care at the Center 2025. Literally, physically, we are all coming together! Join the PFCCpartners community in October for a familiar experience of learning, inclusivity, connection, and inspiration.
- Stephen Hoy
Overview: Together at the Center
As with all things PFCCpartners, the content will feature demonstrations of impactful collaboration between health system partners and people with lived experiences. The essential voices and stories from people’s lived experiences are at the center of these energizing three days.
This partnership will also provide unique co-design events, networking opportunities, workshops, co-design activities, capacity building events such as:
• Dedicated Workshop Track: Partnering with People Who Have Lived-Experience
• PFCCpartners’ Community Networking Event
• Pre-Conference Workshop: The ACT Framework - Initiating Partnerships with Patients, Families, and Communities
• Lived-Experience Luncheon and other networking opportunities for lived-experience partners.
• Key highlights of the people, projects, and transformations happening under Cal-AIM initiatives in California.
• Cultural experiences and immersive learning opportunities about caring for people with complex needs.
Financial assistance, scholarships, and sponsorships will be available for people with lived-experiences.
Call for Proposals are now open! Deadline March 5th.
Have something exciting to share about your work? Learn more and apply today!
What People Value In Their Health Care
What People Value
In Their Health Care
A Guide for Health Plans and Provider Organizations: Understanding the many dimensions of needs that influence what people prioritize when seeking health care services
HCPLAN Person Perspectives Council
The HCPLAN launched the Person Perspectives Council in late 2023 to champion and promote people’s lived experience in the health care system as it relates to the advancement of alternative payment models and value- based care. Council members serve as powerful voices driving their individual missions and increasing the focus on person-centeredness within the HCPLAN and the industry overall.
Current council membership includes representatives from four organizations:
PFCCpartners
Community Catalyst
FamiliesUSA
National Partnership for Women & Families
The business of health care in this country wields enormous power compared to individuals and communities and could be much more intentional about wielding it in ways that protect and enhance everyone’s health. A strong focus on what people say they need and want from the health care system is needed. These findings on person-centered health care priorities can assist entities like health plans, providers, and provider organizations in better achieving a more nuanced understanding of patients’ needs and preferences to improve health outcomes and patient experience in the US. Operationalizing principles can also enhance health organization programmatic and financial strength needed to build healthier communities. Applying the insights of people with lived experience is a critical first step towards adopting practices that improve health outcomes through increased dignity, trust, respect, and ultimately, quality of life.
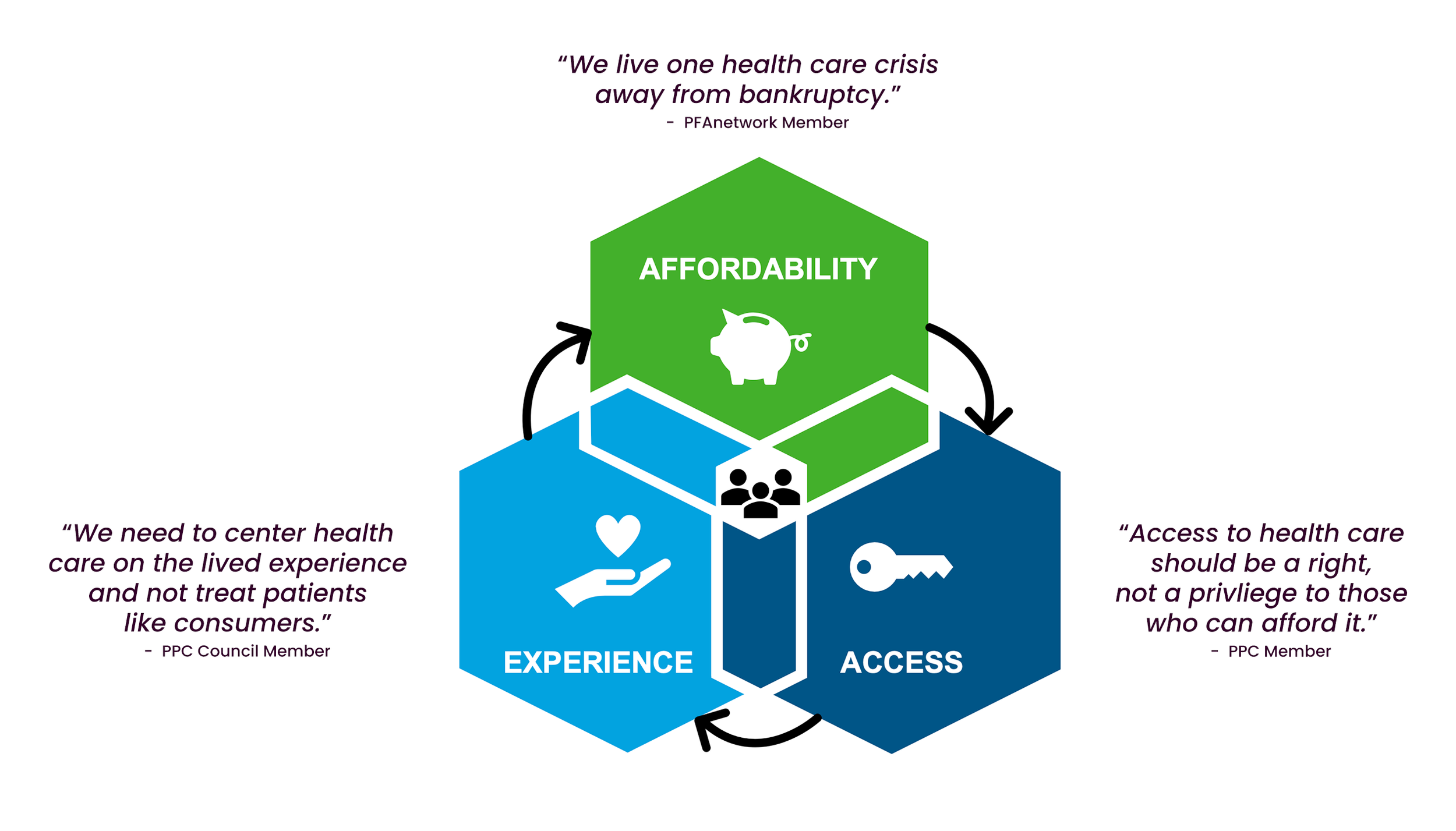
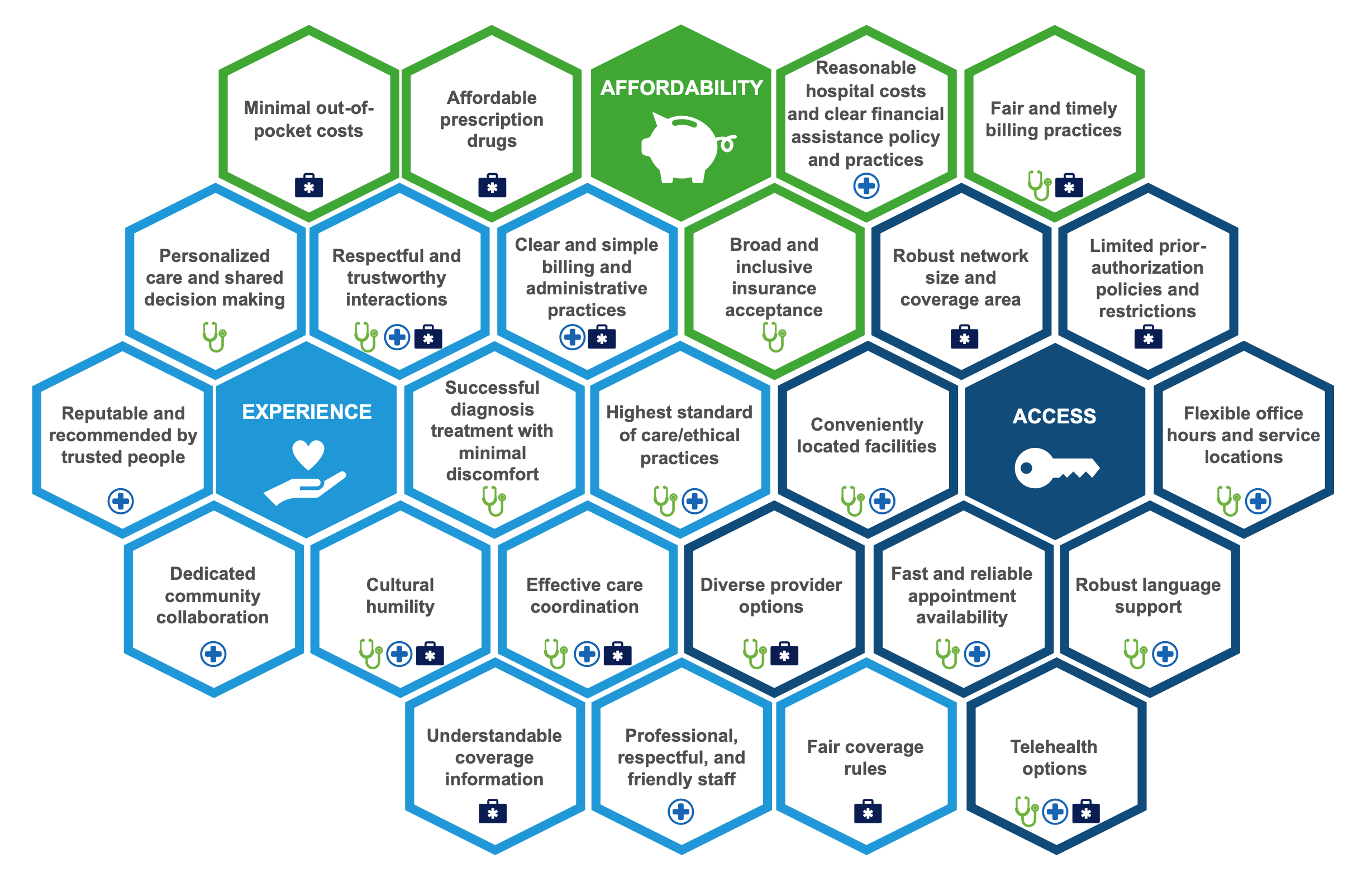
Factors People Prioritize When Seeking Health Care
The Disconnect Between the Industry Today and People’s Priorities
Through assessment of priority dimensions and individual factors, the PPC has identified common sentiments and themes that people hold regarding their health care and about the industry as a whole:
1. Health care costs need to be distributed more fairly to alleviate burdens on people. Many people have difficulty managing health care payments among other financial obligations and feel that too much of the cost burden is falling on people in need of care. This is especially true for out-of-pocket and prescription drug costs; people are unable to afford the cost of care and do not understand why there are such significant cost obligations beyond their regular health coverage contributions. Health industry activation of affordable care strategies is required to ensure health care for all
2. Doctors and services must be placed within reach of more people. People are unsatisfied by the limited health care options available, which too often require travel to distant locations, are offered during work hours, or are not available when people need them. At a minimum, these issues restrict people’s ability to tailor their health care to their personal and lifestyle needs; at worst, people are unable to access critical services altogether. Integrating access enablers into health care models is essential to breaking down current barriers
3. Experience standards and practices should be rooted in people’s needs. While there is general trust in health care providers, many people feel that the system does not account for their needs, does not always respect them, overlooks people’s expectations regarding the quality of their care, and the impact of experiences on health outcomes. Health care entities must adopt programs that measure the quality of the care people receive as well as the quality of their experiences in receiving it.
Disconnects between what people need and prioritize in their health care and what the industry delivers contribute to the underutilization of available high-value health resources and overutilization of more expensive emergency care, exacerbate health and social inequities, and endanger people’s wellbeing. Frank introspection around health organization motivation alignment with the priorities outlined in this assessment must occur to identify existing gaps and eventually develop solutions to provide what people prioritize, for population health prosperity and the fortitude of the health care system. The HCPLAN and Person Perspective Council urge health care leaders to accept these priorities as what people need and adopt them into organizational planning and implementation. Organizations can start by taking the following actions:
• Embrace people’s priorities – deepen your understanding and support organizational recognition of people’s health care priorities. Hold listening sessions with the people you serve to enhance your understanding of their unique needs.
• Understand your population – gain insights into your specific patient population’s needs to tailor application of priorities (e.g., requesting language preference in pre-service questionnaires, translation resources for administrative and clinical staff, etc.)
• Reflect on alignment – are these priorities embedded in the health plan or program design? Is there infrastructure in place to support alignment? Include people as design contributors by hearing from the people you serve about how they see these priorities reflected, or not, in the health plan and program design (e.g., compare current goals and tactical plans to priority factors then, pursue plans that are mutually beneficial)
• Commit to continuous improvement – add accountability to these priorities to organizational infrastructure and use tools to help elicit people’s priorities (e.g., shared decision-making, care coordination advancement, etc.)
Engaging members is a critical driver for transformation!
Get in the water: Authentic community engagement programs meet community members where they are.
There are incredible demonstrations of community engagement happening in health systems around the country, but it takes making mistakes — and learning from them — to get there. Sometimes a well-intended patient focus-group fails to achieve impactful and meaningful engagement, and we have to look internally and say, what do we learn from this? Are we engaging authentically?
Written by: STEPHEN HOY, CHIEF OPERATING OFFICER, PFCCPARTNERS
There are incredible demonstrations of community engagement happening in health systems around the country, but it takes making mistakes — and learning from them — to get there. Sometimes a well-intended patient focus-group fails to achieve impactful and meaningful engagement, and we have to look internally and say, what do we learn from this? Are we engaging authentically?
Understanding what rises to the standard of authentic community engagement is made more challenging when considering that community engagement happens on a spectrum (see spectrum of community engagement). While authentic community engagement can take place at any level of the spectrum, engaging in practices that are not authentic engagement erodes the chances of building a standard for sustained, productive partnerships between community members and the systems we rely on when our bodies and minds are ill.
For a long time, determining what is and isn’t community engagement has been left up to the “sniff” test — like when you open a carton of milk and check for a whiff of something not quite right. Fortunately, new, and evolving measurement systems for community engagement are emerging that can help us finally retire the sniff test. A rule of thumb when considering whether something is or is not community engagement: it is not about whether entities think they are doing a good job engaging communities, but whether communities feel engaged. – National Academy of Medicine.
Getting in the water
Recently, at the beach, I overheard a surfing instructor say to a group of new students, “If you are going to learn to surf, you have to get in the water.” That’s true for community engagement as well. In community engagement, getting in the water means collaborating or learning from people with lived experience (PWLE). If you’re doing that, you’ve already reached a landmark milestone. So often, when health systems are initiating efforts to engage community members, perfection can become the enemy of progress. Just remember, it is easier to learn how to ride a bike when it is moving, and to learn to surf you must get in the water.
From there, advancing your practice is about setting short term goals and monitoring progress. Some enlightening questions we can ask ourselves about community engagement are:
What key decision points are engagement activities supporting?
What do we really need to learn about from community perspectives?
Do our efforts facilitate mutual benefit for our partners with lived experiences?
What are we doing to remove barriers to participation and compensate people for their valuable time and perspectives?
Are we being transparent with our partners, and with ourselves?
Are we doing things for people, or with people?
Do our partners with lived experience have pathways to elevate their priorities in our work together?
When was the last time we were uncomfortable?
What about councils and advisory committees?
In addition to organizations that voluntarily embrace community engagement, several healthcare entities are now required to convene committees of patient, family, or community members often called Patient/Family Advisory Councils (PFACs) or Patient Engagement Committees. Nursing homes are required to facilitate community engagement through Resident Councils, Dual Eligible-Special Needs Plans are contractually obligated to host Enrollee Advisory Committees (EACs), and state Medicaid agencies must maintain Beneficiary Advisory Councils. In short, a lot more people are getting in the water, which is great, but there are some common challenges with the council and committee approach.
First, we must recognize that volunteerism is a privilege and many of these committees do not provide monetary compensation to their members. Many of these councils fail to engage groups that represent the diversity of backgrounds present within the community being served — and therefore fall short in hearing the voices and perspectives that have the most to teach us about providing good healthcare. Many committees focus their time on limited conversations about individual experiences and minor issues — like facility decor and amenities — when there are far greater collaboration opportunities and discussions to have such as the safety, quality, and equity of care.
The trick to making these committees meaningful lies in agenda setting and facilitation of patient-centered co-design. The best examples of these committees:
Feature shared leadership with PWLE, often in a role like Co-Chair.
Set discussion topics that integrate staff from the organization’s priority projects to seek meaningful and actionable feedback from committee members.
Establish avenues for elevating the priorities and key concerns of members.
Make huge efforts to ensure people can participate by overcoming barriers such as transportation, time/location of meetings, accessibility and language access.
Build members’ confidence for participation by providing orientation and ongoing support.
Community engagement doesn’t have to be relegated to just stand-alone committees of PWLE. Many organizations find that a more impactful approach is engaging PWLE as advisors to existing internal committees or within specific operational units (e.g. equity committees, office of patient experience, quality departments). Here insights from PWLE may be more easily aligned to support key decision points about priority health challenges, inequities, and community needs.
Finally, thinking back to the spectrum of community engagement, it is also important to remember that community engagement doesn’t have to happen behind the walls of a clinic or hospital — it can (and probably should) also happen in coffee shops, community health fairs, listening sessions, and in partnership with community-based organizations.
Sour whiffs
Some examples of weak or limited engagement, so we all have a chance to learn and grow:
Marketing activities that are used only to promote the organization.
Engagement with a high bar for entry such as conducting background checks, holding meetings only during standard business hours, or failing to address issues of accessibility
Checkbox, token engagement that only brings PWLE in for a final “sign off” and fails to meet any criteria for being authentic in terms of diversity, impact, integration, etc.
Misconstruing community engagement for other (worthy, but different) activities like forming partnerships with other organizations and health education/promotion activities.
Beyond the sniff test
Getting in the water, and meeting the community where they are, is the pillar from which to build an authentic community engagement program. And now there’s a roadmap for how you get in there.
The project of defining and implementing authentic community engagement has made a massive leap forward with the publication of “A roadmap for effective community engagement in healthcare,” a new report from the INSPIRE project. The report synthesizes a year of research into both a snapshot of the current state of community engagement in healthcare and a set of recommendations for how healthcare leaders and staff, PWLE, policymakers, and more can move forward together.
I was honored to be a part of the team that put this roadmap together. And we’re not done yet – the next phase of INSPIRE will be to create tools that help turn the vision we laid out into a reality. Stay tuned!
INSPIRE Report: A Roadmap to Authentic Community Engagement
INSPIRE (Initiating National Strategies for Partnership, Inclusion, and Real Engagement) is a collaborative and coordinated team of organizations and people with lived experience committed to advancing the practice of authentic community engagement in the U.S. healthcare system.
A roadmap for effective community engagement in healthcare: Final report from INSPIRE Phase 1
INSPIRE (Initiating National Strategies for Partnership, Inclusion, and Real Engagement) is a collaborative and coordinated team of organizations and people with lived experience committed to advancing the practice of authentic community engagement (CE) in the US healthcare system.
Phase 1 of INSPIRE consisted of a year-long research and strategic planning phase that included collecting feedback from 300 individuals across sectors and the nation. Activities included several listening sessions, targeted literature analysis, key informant interviews, and a field survey.
The resulting report provides a roadmap for how healthcare organizations and people with lived experience can realize the full potential of authentic CE to build trust, advance health equity, create cost-savings and efficiencies, and create healthy and thriving communities. From compensating people with lived experience to creating trauma-informed spaces, learn how you can build stronger connections, get genuine feedback, and advance equity in your community.
Additional supplementary materials:
Moving toward meaningful community engagement: A targeted literature analysis
Making the “business case” for sustained investment in community engagement
Our goal is for the roadmap and recommendations in the report to be implemented across the country. Use our toolkit to share the report with your colleagues, organizational leadership, partners, and network.
INSPIRE Core Organizations
Partnering People With Lived Experience
PFCCpartners Knowledge Cafe Report
People with Lived-Experiences (PWLE) have essential perspectives on how to successfully screen for and address social drivers of health in the health system. Discover what expressed challenges and knowledge is gleaned from our person-centered, multi-stakeholder collaboration events.
People with Lived-Experiences (PWLE) have essential perspectives on how to successfully screen for and address social drivers of health in the health system. Discover what expressed challenges and knowledge is gleaned from our person-centered, multi-stakeholder collaboration events. Click the button below to dive into our comprehensive report.
“If we don’t take a person-centered approach to SDOH screening, we risk conveying that improving our data is a priority over authentically supporting people’s social needs.” - Stephen Hoy, PFCCpartners
Meet PFCCpartners’ NEW TEAM MEMBER!
It is with great excitement that we introduce Brittany Jackson as the newest addition to the PFCCpartners family, stepping into the vital role of Community Connection Coordinator. With a wealth of experience and a passion for community engagement, Brittany brings a delightful energy to our team.
Greetings everyone,
It is with great excitement that we introduce Brittany Jackson as the newest addition to the PFCCpartners family, stepping into the vital role of Community Connection Coordinator. With a wealth of experience and a passion for community engagement, Brittany brings a delightful energy to our team.
In her capacity, Brittany will be instrumental in cultivating impactful partnerships and fostering collaborative efforts that empower individuals with lived-experiences to catalyze change. Her dedication to building strong connections aligns perfectly with our mission to authentically engage patients, family caregivers, and community voices.
We look forward to Brittany's contributions in expanding the reach of our PFAnetwork Community and creating impactful change within healthcare and beyond. Please join us in extending a warm welcome to Brittany as she embarks on this journey with us.
The PFCCpartners Team
MEET BRITTANY JACKSON
Brittany has a passion for people; she works to foster relationships, care for people, grow capacity, and encourage empathy to strengthen the healthcare system. Brittany has lived through various encounters with the healthcare system, both as a patient and family support partner. She is a facilitator, convener, and coach and has done valuable work with quality improvement staff, health care professionals, clinicians, dually eligible individuals, and older adults across the country utilizing and spreading the tactics of community organizing, coaching, adult learning techniques, and leadership development. She has extensive experience in gathering and spreading best practices and results-oriented approaches to catalyze overall quality improvement on a local and national scale.
Brittany has a Master’s Degree in Adult Education: Adult Learning, Training & Development, and uses her skills towards the ongoing improvement of health care quality. She has dynamic communication, relationship building, facilitation, strategic and forward-thinking skills.
Brittany lives in Colorado and enjoys spending quality time with her family, painting, baking bread, crocheting, and relaxing in nature.
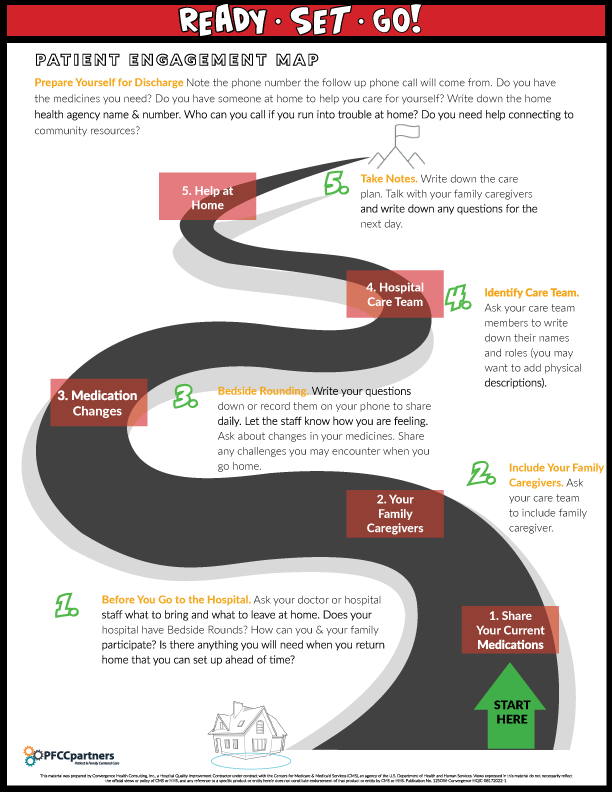
Ready, Set, Go!
Ready, Set, Go! was co-designed by hospital staff and Patient Family Partners in partnership with HQIC to address and connect the critical processes that take place between admission planning, bedside rounding, and discharge planning in an effort to reduce hospital readmissions.
Ready, Set, Go! was co-designed by hospital staff and Patient Family Partners in partnership with HQIC to address and connect the critical processes that take place between admission planning, bedside rounding, and discharge planning in an effort to reduce hospital readmissions. This new resource includes key insights into the three processes plus 5 embedded tools to enhance current processes at the hospital.
Are you ready to get started connecting these three activities to improve patient outcomes and avoid readmissions? The tool also includes implementation guidance to support hospitals ready to take action using Ready, Set, Go!
Are we speaking the same language?
Shared language is an essential element of meaningful community engagement.
Shared language is an essential element of meaningful community engagement. This should come as no surprise. It can look like:
Having an interpreter and translated materials for people who speak languages other than English
Prioritizing digital accessibility
Avoiding “insider lingo” and jargon that can be a challenge for community members and organizational staff alike to understand
Coming to a shared understanding of what we mean by “value” in healthcare
Importantly, shared language is also about having a common understanding of what we even mean by “community” and “community engagement.”
INSPIRE (Initiating National Strategies for Partnership, Inclusion, and Real Engagement), has brought together a national team committed to advancing partnerships between healthcare organizations and people with lived experiences across the country. Creating shared language is an important first step toward ensuring that we can communicate with one another about our community engagement work, goals, and challenges — and can hold one another accountable to building authentic, mutually beneficial partnerships.
Who is "community?"
Community can refer to people who live in the same geographic area and/or people who have characteristics or experiences in common. INSPIRE refers to individuals within a community as “community members” or “people with lived experience.” Community can also refer to organizations that serve people within a shared geographic area and/or that have a common service focus. Some organizations are representative of and/or led by community members themselves, and some are not.
Some notes about defining “community:”
The way people identify their own community affiliations may be different than the way healthcare organizations identify community affiliations. For instance, healthcare organizations may think of people as “Medicaid recipients”, while they may think of themselves as a member of a specific health plan/managed care organization — or not define themselves based on their health insurance status at all.
Some people say “but we all have lived experience.” While this is true, factors such as race, class, geography, and identity drive significant differences in how individuals and communities can or cannot access high-quality and person-centered healthcare. INSPIRE is focused primarily on ensuring that people and communities who are impacted by structural racism, injustices, and health disparities have opportunities to engage and partner with the systems and organizations endeavoring to serve them.
What is “community engagement?”
Source: simplystakeholders.com
Community engagement refers to the different ways in which healthcare organizations can reach out to, engage, and partner with people with lived experience, with the goal of working together to improve healthcare and achieve positive health outcomes.
Like the definitions of community engagement from WHO and CDC, ours highlights concepts of relationships, collaboration, and outcomes. We also prioritize creating a plain language definition that is accessible across invested parties.
Community engagement can be focused on working with people with lived experience and/or with other organizations in the community. An early observation of our team is that healthcare organizations are most often thinking about and undertaking community engagement with organizations. INSPIRE, however, is focused on improving direct engagement/partnerships with people with lived experience.
What can community engagement look like?
Source: vcccalliance.org.au
Community engagement models provide a framework for considering the degree to which community members and people with lived experiences are engaged and centered in the process. The above diagram, created by the VCCCC Alliance, shows a spectrum of community engagement approaches, from informing to consulting to involving to partnership to consumer-led. Several other variations of community engagement spectrums exist with slightly different ways of categorizing or defining engagement approaches.
A core tenet of INSPIRE’s work is that people with lived experience must have opportunities to partner with organizations in ways that go beyond informing and consulting. To achieve healthcare’s goals of improved outcomes in cost, quality, and access, and to advance health equity, community involvement, partnership, and leadership are necessary.
Healthcare organizations should thus prioritize robust opportunities for partnership by ensuring that people with lived experience are centered-in and leaders of the work. Offering multiple engagement opportunities across the spectrum ensures that all people with lived experience have the opportunity to participate in ways that meet their interests, abilities, and needs.
A step toward shared language
INSPIRE is working to harness the growing interest in community engagement in healthcare while also addressing the need for real-world support and guidance on how to actually do the work in authentic and impactful ways. Developing a shared language and common understanding of how we define and understand community engagement is an important first step.
While healthcare continues to make advances in organizational level community partnerships, more attention is needed to building partnerships with organizations that are truly representative of the communities they serve – and building partnerships with people with lived experiences themselves.
In the coming months, INSPIRE will be undertaking a research and strategic planning phase to summarize the current state of community engagement work in healthcare, identify the desired future state based on best practices and key opportunity areas, and, most importantly, create a roadmap for how the field can close this gap. We hope to connect with many healthcare stakeholders and people with lived experience in the process and welcome you to reach out to us.
Please contact Taylor Brown at tbrown@camdenhealth.org with questions about the project or interest in getting involved.
Partnering Organizations
LEARN ABOUT THE INSPIRE PROJECT
We are seeking to gain better understanding about how community engagement is currently impacting different elements of the health care system. We would like to hear from ANYONE WORKING IN A HEALTHCARE ORGANIZATION!
ABOUT THE INSPIRE PROJECT
ISSUE
Building impactful, equitable, and mutually beneficial partnerships with community members and people with lived experience (PWLE) is an ethical imperative for healthcare. While there has been growing interest among healthcare organizations to engage community members and PWLE, many lack clear best practices for building and sustaining these partnerships.
PROJECT GOAL
Develop a national strategy for authentic community engagement in healthcare and create tools, resources, and learning and coaching models that will meet the varied needs of healthcare stakeholders and PWLE to advance meaningful partnerships in their communities.
BACKGROUND
The Camden Coalition, the Commonwealth Care Alliance and its Center to Advance Consumer Partnership, PFCCpartners, the Institute for Patient and Family Centered Care, and Community Catalyst are all national organizations deeply committed to advancing partnerships with community members/PWLE.
Our collective work includes building meaningful community partnerships within our own organizations as well as supporting the growth of healthcare organizations’ capacity to build and sustain their own community engagement work.
We are able to do this work due to the relationships we each have with community members/PWLE.
Community engagement and partnership work with PWLE has always been a core value of the Camden Coalition. To ensure that health and social care programs understand, respond to, and meet the needs of individuals and their communities, we believe that PWLE must be equal partners in the work.
Several important advancements in the national community engagement landscape have been important precursors for this project. In 2022, the National Academy of Medicine (NAM) released “Assessing meaningful community engagement: A conceptual model to advance health equity through transformed systems for health” (NAM, 2022), the first product to come from their extensive work with a national expert Organizing Committee. In addition, the Center for Medicare and Medicaid’s announced a new requirement for health insurance companies that offer Dual Eligible Special Needs Plans (plans that serve people eligible for both Medicare and Medicaid) to establish and maintain an enrollee advisory committee (Hafner and Fish, 2022).
Given the significance of these new resources and requirements, there is a window of opportunity to support the healthcare field by identifying and codifying the best practices for building community partnerships, as well as by creating tools and resources for organizations and community members/PWLE to translate these practices into action — together.
PROJECT DESIGN
This project, which we are calling INSPIRE (Initiating National Strategies for Partnership, Inclusion, and Real Engagement) will include two phases: Phase 1 will involve a 12-month strategic planning and research period during which the Core Team will collectively:
Assess the current state of community engagement work nationwide
Identify best practices through a series of focus groups and/or interviews with key stakeholders including PWLE who are engaged in work as advisors/advocates
Articulate a value proposition for community members/PWLE to become engaged in this work
Create a business case/financial framework for partnerships between healthcare and community members/PWLE, including identification of reimbursement pathways to support the financing and sustainability of such work for organizations
At the end of phase 1, we will produce a comprehensive report that summarizes the current state of community engagement work in healthcare, the desired future state based on identified best practices and key opportunity areas, and, most importantly, a roadmap for how the field can close this gap — including the financial and policy levers that can create accountability and incentives for adoption of this work across healthcare.
In phase 2 of this project, we hope to focus on translating phase 1 findings and outputs into tangible products and opportunities to drive widespread adoption of effective community engagement and partnership strategies across healthcare.
These may include toolkits, implementation tools, case studies, learning communities, and targeted technical assistance offerings and training products. The content of these will be determined by our findings in phase 1.
This project launches in May 2023, with phase 1 concluding in April 2024.
PARTNERING ORGANIZATIONS
PARTNERING PEOPLE WITH LIVED EXPERIENCE
NEW TOOL! Milestone Moments Template
Celebrating successes are important in patient/family engagement (PFE), as in any long journey! Even small milestones deserve celebration. Use this new template to capture your PFE milestones!
Impactfully engaging patients and family caregivers is a journey with many milestones along the way. Celebrating those milestones help teams visualize progress and advance practice.
We invite you to use this template to record your PFE milestones and share your completed template with us - so we can celebrate with you!
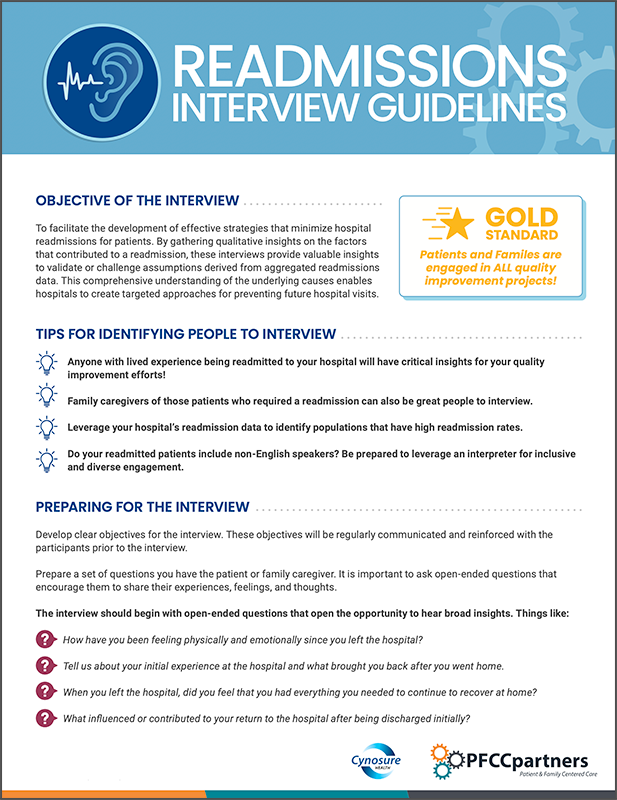
NEW TOOL! Readmissions Interview Guidelines
Short conversations with your patients and family caregivers unlock the core factors that are contributing to hospital readmissions. Their valuable insights can validate or challenge assumptions based on aggregated readmissions data. Anyone on your team can use this guide to feel confident organizing and facilitating a readmissions interview.
Short conversations with your patients and family caregivers unlock the core factors that are contributing to hospital readmissions. Their valuable insights can validate or challenge assumptions based on aggregated readmissions data. Anyone on your team can use this guide to feel confident organizing and facilitating a readmissions interview.
A Patient-Centered Complex Care Research Agenda
I am proud to announce PFCCpartners was recently a project partner on the development of the Patient-Centered Complex Care Research Agenda.
Hello everyone!
I am proud to announce PFCCpartners was recently a project partner on the development of the Patient-Centered Complex Care Research Agenda. PFCCpartners led the engagement activities for the project, and sincerely thank each of the patient and family caregivers who partnered on this project.
The Research Agenda outlines three core strategies and corresponding action steps to build a stronger, more coordinated, and patient-centered complex care evidence base.
1. Meaningfully Partner With Patients and Communities in Research
2. Focus on a Prioritized Set of Research Questions
3. Measure Outcomes in a More Consistent and Patient-Centered Way
I would like to personally invite you to review the Research Agenda and the recording of our September Community of Practice Workshop discussing its development.
Stephen Hoy
PFCCpartners, Chief Operations Officer
About the PFCCpartners and CHCS collaboration
"Nothing about us without us" became the motto during the monthly Patient Family Advisory Board (PFAB) planning and workgroup meetings. The group that worked on this project showed theory in action through active participation and listening, transparency, hard conversations and discussions that ended with meaningful resolutions. True collaboration was born was challenging questions and intense dialogue.
CHCS was committed to bringing and including the voices and what matters most of the lived experience experts. This can be seen in the research agenda recommendations, most pronounced with the measurement domain.
As the liaison on this project, it was refreshing to see every person involved have an "ah ha" growth moment.
Naomi Williams
Patient Family Engagement Specialist, PFCCpartners
A Patient-Centered Complex Care Research Agenda
"A guide to build the complex care evidence base by prioritizing what matters most to people with complex health and social needs."
ABOUT THE RESEARCH AGENDA
Success in complex care programs has traditionally been defined by reductions in health care costs or unnecessary utilization and not by what matters most to patients. There is much more for complex care to learn about which services work best for which groups of people and how it can best support patient goals.
Recognizing this need, the Center for Health Care Strategies (CHCS) developed the Patient-Centered Complex Care Research Agenda with funding from the Patient-Centered Outcomes Research Institute. The Research Agenda was co-created by more than 100 partners, including patients with lived expertise of complex care, researchers, providers, and health care system leaders.
ABOUT CHCS
The Center for Health Care Strategies (CHCS) is a policy design and implementation partner devoted to improving outcomes for people enrolled in Medicaid. We connect people and ideas to spark insights, build expertise, strengthen leadership, and spread innovations. CHCS works to improve health outcomes for the millions of people in the U.S. who face serious barriers to well-being, like poverty, complex health and social needs, and systemic racism.
Lessons Learned from Engaging People with Lived Experience to Inform Complex Care Research
Presented by:
Naomi Williams
Patient Family Engagement Specialist, PFCCpartners
RECORDED: Friday, September 30
Watch this month's PFCCpartners Community of Practice Workshop to learn about our recent collaboration with the Center for Health Care Strategies (CHCS). PFCCpartners supported the development of their Patient Family Advisory Board (PFAB) to be engaged throughout the development of the CHCS Research Agenda. The CHCS PFAB includes people with complex health care needs (including medical, mental health and/or substance use conditions) and social needs (e.g., housing, food access, and transportation).
PFCCpartners Readiness Tool
This tool is built on the successes and failures of hundreds of teams who have already begun engaging patient and family caregiver voices. Get ready to engage now – and bring this essential voice into your efforts to improve.
There are two main ingredients for successfully launching a patient/family partnership program: commitment and resource. But what resources are needed to get started? And what commitments are essential for authenticity, inclusivity, and constructive collaboration?
Whether your re-booting or starting a new partnership program - our newly released Readiness Tool will prepare your organization or team for impactful collaborations with your community members.
This tool is built on the successes and failures of hundreds of teams who have already begun engaging patient and family caregiver voices. Get ready to engage now – and bring this essential voice into your efforts to improve.